Is MS hereditary? No, multiple sclerosis (MS) is not directly inherited in the way conditions like cystic fibrosis are. There is no single “MS gene,” and doctors do not classify MS as a strictly hereditary disease. However, MS does have a genetic component, which means family history can slightly increase a person’s risk.
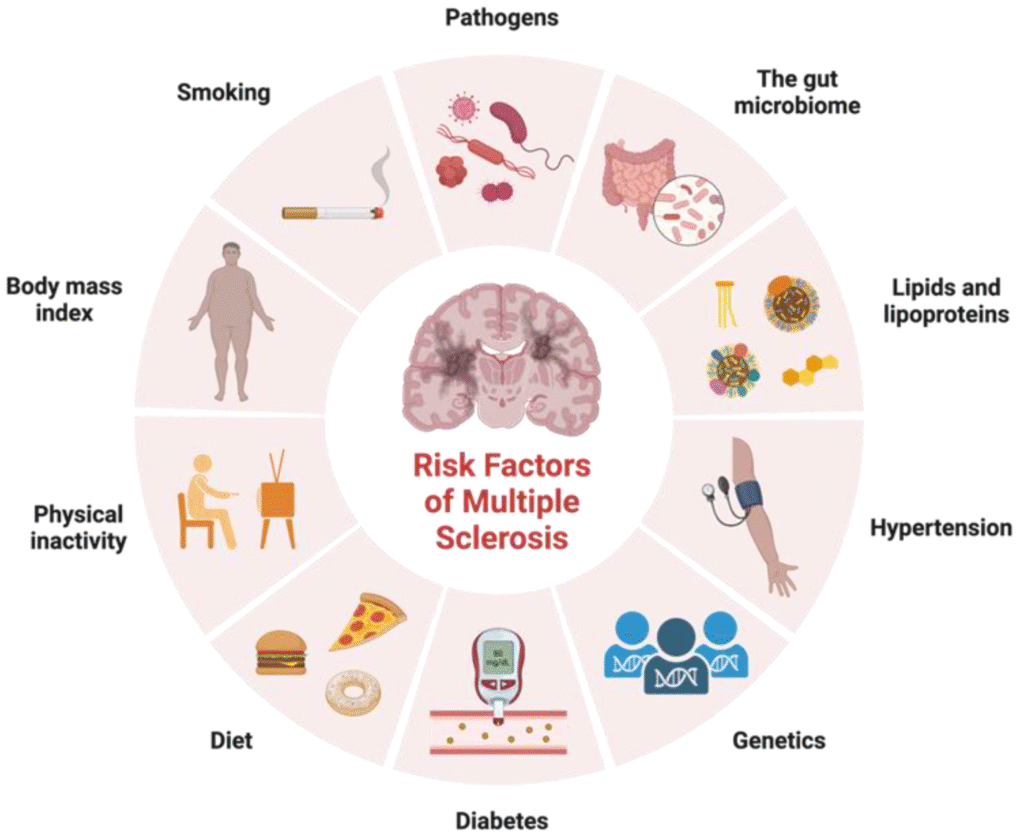
More than 200 gene variations may influence susceptibility, especially genes linked to the immune system. But genes alone do not cause MS. Environmental factors such as Epstein-Barr virus infection, low vitamin D levels, smoking, and obesity appear to interact with genetic risk to trigger the disease.
So while MS can run in families, it is not a guaranteed inherited disease. Most people diagnosed with MS have no family history of the condition.
Can MS Be Passed From Parent to Child?
Many families ask, can MS be passed from parent to child? The answer is reassuring: the risk remains low.
If one parent has MS, a child has roughly a 1.5% to 2.5% chance of developing it. That means more than 97 out of 100 children of a parent with MS will not develop the condition. MS does not follow a predictable inheritance pattern, and doctors do not consider it a directly inherited disease.
Is MS Hereditary From Mother?
Some caregivers worry specifically, is MS hereditary from mother? Research shows that the risk does not significantly differ whether the parent with MS is the mother or the father. What matters is the shared genetic background, not which parent carries the condition.
Is MS Hereditary From Grandmother?
The risk becomes even smaller across generations. If a grandparent has MS, the increased risk to grandchildren is very slight. MS does not “skip generations” in a classic genetic sense. It reflects inherited susceptibility combined with environmental exposure, not a guaranteed transmission line.
What About Siblings and Twins?
If a brother or sister has MS, the lifetime risk rises slightly to around 2–3%. Identical twins share the same genetic material, yet if one twin has MS, the other develops it only about 20–30% of the time. This strongly supports the idea that genes increase vulnerability, but they do not act alone.
For caregivers and families, the key message is this: having MS in the family increases risk modestly, but it does not mean children or relatives will develop the disease.
READ MORE: Employment Rights Bill: What UK Care Workers Must Do Before 2026–2027
What Causes Multiple Sclerosis?
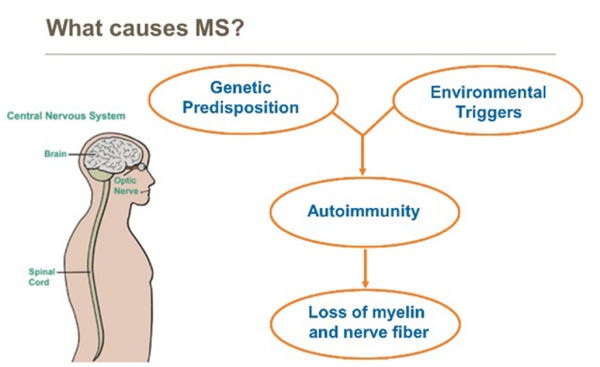
If MS is not directly inherited, then what causes MS? Researchers believe multiple sclerosis develops when genetic susceptibility interacts with environmental triggers. No single cause explains every case.
MS begins when the immune system mistakenly attacks myelin, the protective covering around nerve fibres in the brain and spinal cord. This damage disrupts communication between the brain and the body. Scientists still study why this immune misfire happens, but several risk factors consistently appear in research.
Genetic Susceptibility
Certain gene variations, particularly those involved in immune regulation, increase the likelihood of developing MS. These genes do not guarantee the disease. Instead, they make the immune system more likely to react abnormally under certain conditions.
This helps explain why MS sometimes appears in families but does not follow a clear inheritance pattern.
Environmental Triggers
Environmental exposure plays a crucial role in triggering MS in genetically susceptible individuals. The strongest factors include:
- Epstein-Barr virus (EBV): Nearly all people with MS show prior EBV infection. Researchers consider EBV a major risk factor, though it does not cause MS on its own.
- Low vitamin D levels: MS occurs more frequently in regions further from the equator, including the UK. Reduced sunlight exposure may influence immune regulation.
- Smoking: Smoking increases the risk of developing MS and can worsen disease progression.
- Childhood or adolescent obesity: Higher body fat levels may increase inflammation and immune dysregulation.
What Causes Multiple Sclerosis in Females?
MS affects women about two to three times more often than men. Researchers believe hormones, particularly estrogen and progesterone, influence immune system behaviour. Female immune systems generally mount stronger immune responses, which may increase susceptibility to autoimmune conditions like MS.
However, scientists have not identified a single explanation. Genetics, hormones, and environmental exposures likely work together.
For caregivers, the most important takeaway is this: MS develops from a complex interaction between genes and environment, not from one single inherited cause.
SEE ALSO: How a Domiciliary Care Agency Can Prepare (2026)
How Is MS Diagnosed?
Families often ask about MS diagnosis and whether a single MS test can confirm the condition. Doctors do not rely on one standalone test. Instead, they combine clinical evaluation with imaging and laboratory findings to confirm multiple sclerosis.
There Is No Single “MS Test”
You cannot confirm MS with a routine blood test. Doctors must show that damage has occurred in different parts of the central nervous system at different times. This principle is called “dissemination in space and time.”
MRI Scans
An MRI scan plays a central role in muscular sclerosis testing, although the correct term is multiple sclerosis testing, not muscular sclerosis. MRI images can reveal lesions or scars in the brain and spinal cord that indicate immune-related damage to myelin.
Lumbar Puncture (Spinal Tap)
Doctors may perform a lumbar puncture to examine cerebrospinal fluid. The presence of certain immune proteins, called oligoclonal bands, can support an MS diagnosis.
Additional Tests
Neurologists may also use:
- Evoked potential tests to measure nerve signal speed
- Blood tests to rule out other neurological conditions
Why Early Diagnosis is Important
Early diagnosis allows treatment to begin sooner. Disease-modifying therapies can reduce relapse frequency and slow progression, especially in relapsing forms of MS.
For UK families, the MS NHS pathway typically begins with a GP referral to a neurologist. If you notice persistent neurological symptoms, seek medical advice promptly rather than relying on online tools or self-assessment.
Types of MS Explained
Understanding the types of MS helps caregivers anticipate how the condition may progress. Doctors classify MS based on how symptoms appear and change over time.
Relapsing-Remitting MS (RRMS)
This is the most common form. People experience clearly defined attacks (relapses) followed by periods of partial or complete recovery (remission). During remission, symptoms may improve significantly or disappear.
Secondary Progressive MS (SPMS)
Many people who start with relapsing-remitting MS later develop secondary progressive MS, sometimes shortened in searches as “MS and second.” In this stage, disability gradually worsens over time, even without clear relapses.
Primary Progressive MS (PPMS)
In this type, symptoms steadily worsen from the beginning without distinct relapses or remissions. It affects men and women more equally than relapsing forms.
Clinically Isolated Syndrome (CIS)
CIS describes a first neurological episode that resembles MS but does not yet meet full diagnostic criteria. Some people with CIS later develop MS, while others do not.
Each type behaves differently. Early identification allows neurologists to choose the most appropriate treatment strategy and monitoring plan.
LEARN MORE: Zero Hour Agreement in UK Care: How to Stay Compliant (2026)
Is MS Fatal?
Many families ask directly, is MS fatal? In most cases, the answer is no.
Multiple sclerosis rarely causes death on its own. Most people with MS live close to a normal life expectancy. However, severe disability over time can increase the risk of complications such as infections, swallowing difficulties, or reduced mobility, which may indirectly affect long-term health.
Modern treatments have significantly improved outcomes. Disease-modifying therapies reduce relapse frequency and may slow progression, especially when doctors start treatment early. Better symptom management, rehabilitation, and specialist care have also improved quality of life.
It is important to understand that MS varies widely. Some people experience mild symptoms for decades. Others develop progressive disability. Doctors cannot predict the exact course at diagnosis.
For caregivers, the key takeaway is this: MS is a chronic neurological condition, but it is not usually fatal. Early diagnosis, specialist care, and lifestyle management make a meaningful difference.
Early Symptoms of MS in Women and Men
Recognising early warning signs helps families seek timely medical advice. Symptoms vary, but they often appear suddenly and may improve before returning.
Early Symptoms of MS in Women
Women develop MS more often than men, and early symptoms can include:
- Persistent fatigue that does not improve with rest
- Numbness or tingling in the face, arms, or legs
- Vision problems, such as blurred or double vision
- Weakness in one side of the body
- Balance or coordination difficulties
Some women notice that symptoms worsen around hormonal changes, including pregnancy or their MS period cycle. Fluctuating hormones may temporarily intensify fatigue or sensory symptoms.
Men With MS Symptoms
Men with MS symptoms often experience:
- Progressive stiffness or muscle weakness
- Walking difficulties
- Vision disturbances
- Bladder dysfunction
Men may present more frequently with progressive forms of MS, although this varies between individuals.
What Is the “MS Hug”?
The MS hug describes a tight, squeezing sensation around the chest or abdomen. Muscle spasms in the rib area cause this symptom. It can feel alarming but does not usually signal heart problems. However, anyone experiencing chest pain for the first time should seek urgent medical advice to rule out other causes.
Symptoms often appear in episodes and then partially improve. If neurological symptoms last longer than 24 hours without explanation, consult a GP for referral.
Early recognition supports faster MS diagnosis and earlier treatment intervention.
ALSO: How to Choose Home Care Agencies in the UK (2026)
Is There an MS Risk Calculator?
People often search for an MS risk calculator to estimate their personal chances of developing multiple sclerosis. At present, no clinically validated public calculator can accurately predict who will develop MS.
Doctors assess risk based on known factors, including:
- Family history
- Prior Epstein-Barr virus infection
- Smoking history
- Vitamin D levels
- Obesity during childhood or adolescence
- Biological sex
Even when several risk factors are present, MS remains uncommon. For example, having a parent with MS increases lifetime risk only slightly, and most children of parents with MS never develop the condition.
Genetic testing does not provide definitive answers. Researchers have identified over 200 gene variants associated with susceptibility, but no single gene confirms or rules out MS. For this reason, doctors do not use genetic screening as a routine MS test.
If you worry about your risk, speak with a healthcare professional rather than relying on online tools. A clinician can evaluate your history, explain realistic risk levels, and recommend monitoring only if necessary.
The most important message remains consistent: MS develops from a combination of factors, not from one predictable inherited pathway.
Does MS Affect Periods or Hormones?
Many women ask whether MS interacts with hormones or affects the menstrual cycle. While MS does not directly cause irregular periods, hormonal changes can influence how symptoms feel at certain times of the month.
Some women report that fatigue, weakness, or sensory symptoms temporarily worsen just before or during their MS period. Fluctuations in estrogen and progesterone may affect immune activity, which can intensify symptoms without causing new disease activity.
Pregnancy often reduces relapse rates, especially in the second and third trimesters, likely due to hormonal and immune system shifts. However, relapse risk may increase in the months after delivery.
MS itself does not cause infertility, and most women with MS can conceive and carry a pregnancy safely with proper medical guidance. Neurologists may adjust medications before conception to ensure safety.
If symptoms consistently worsen around menstruation, discuss this pattern with a specialist. Doctors can suggest symptom management strategies and review treatment plans if necessary.
Hormones influence symptom expression, but they do not change the underlying genetic risk of developing MS.
READ: New Rules for Care Home Payments in 2026
What This Means for Families and Caregivers
If you searched “is MS hereditary”, you likely worry about someone you love. The evidence should offer reassurance.
MS is not directly passed from parent to child. It does not follow a predictable inheritance pattern. While family history slightly increases risk, the overall likelihood remains low. Most people diagnosed with MS have no close relatives with the condition.
Understanding this helps caregivers focus on what truly matters:
- Recognise early neurological symptoms.
- Encourage prompt medical evaluation.
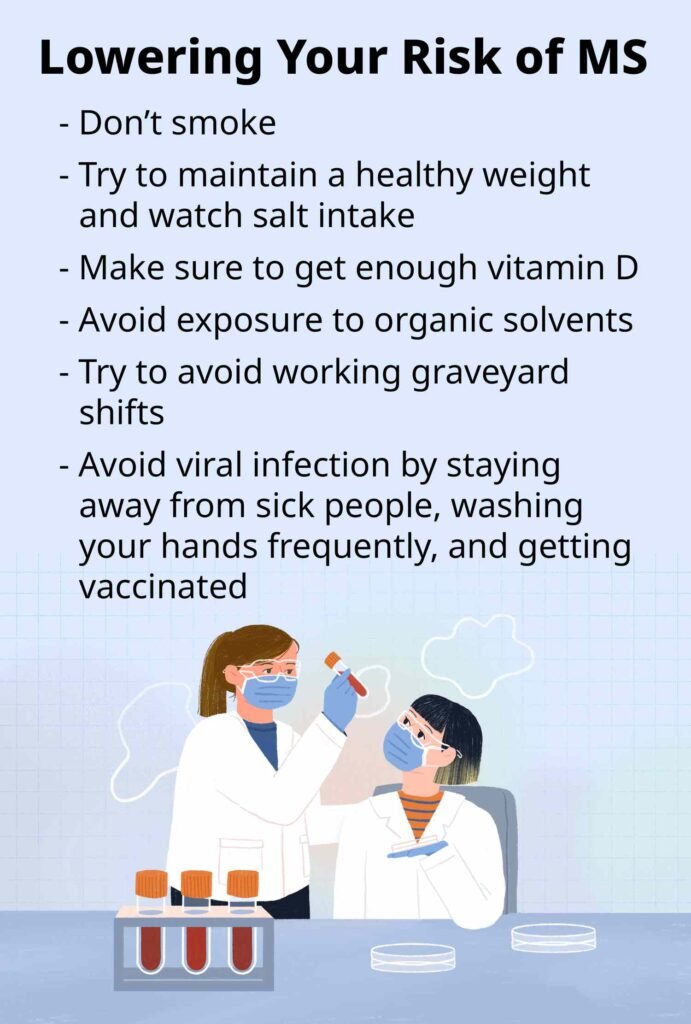
- Support healthy lifestyle choices such as avoiding smoking and maintaining adequate vitamin D levels.
- Stay informed through trusted sources such as the MS NHS guidance and specialist clinics.
MS develops from a complex interaction between genes and environment, not from a single inherited defect. You cannot “test away” the uncertainty, and no MS risk calculator can give a guaranteed answer. But you can respond early, seek expert advice, and support informed care decisions.
For families, the key takeaway remains clear:
MS has a genetic component, but it is not a straightforward hereditary disease. Risk increases slightly within families, yet it does not determine destiny.
Final Thoughts…
When families ask, “Is MS hereditary?”, they are rarely asking out of curiosity. They are asking out of concern, for their children, their siblings, or themselves.
The science gives a balanced answer. MS has a genetic component, but it is not a straightforward inherited disease. Family history slightly increases risk, yet most people with a parent or sibling who has MS will never develop it. Identical twins do not even share certainty. Genes influence vulnerability, they do not write fate.
What truly shapes MS risk is complexity. Immune system genetics, viral exposure, vitamin D levels, smoking, hormonal influences, and environmental factors all interact in ways researchers still study. That complexity explains why MS cannot be predicted by a simple test, a single gene, or an online calculator.
For caregivers and families, this perspective matters. Instead of focusing on fear of inheritance, focus on awareness. Recognise early neurological symptoms. Encourage medical evaluation when something feels persistently wrong. Support healthy lifestyle habits that reduce modifiable risks. Stay informed through credible medical sources.
MS remains a serious neurological condition, but it is not a guaranteed legacy passed through generations. Risk increases slightly within families, yet it does not determine the future.
Understanding that difference empowers families to replace anxiety with informed action.
Concerned About MS Risk in Someone or Persons You Care For?
If you searched “is MS hereditary”, you are likely thinking about someone you care for, or your own long-term health.
Clear, accurate information matters. Misunderstanding risk can cause unnecessary fear, while missing early symptoms can delay diagnosis and treatment.
Care Sync Experts supports families, caregivers, and care providers across the UK with:
- Clear interpretation of NHS and specialist MS guidance
- Education sessions for domiciliary care and supported living teams
- Early-symptom awareness training for frontline staff
- Care planning frameworks for clients living with MS
- Risk communication support for families worried about hereditary conditions
- Governance guidance aligned with neurological care best practice
- Policy development for managing progressive neurological conditions in care settings
- Referral pathway mapping to ensure timely GP and neurology access
Whether you support someone newly diagnosed, manage a domiciliary care agency, or oversee supported living services, we help you move from uncertainty to informed action.
Get in touch with Care Sync Experts today and ensure your care systems are prepared, proactive, and grounded in evidence, not fear.
FAQ
What Does MS (Multiple Sclerosis) Mean?
Multiple sclerosis (MS) is a chronic autoimmune condition that affects the central nervous system, the brain and spinal cord. In MS, the immune system attacks myelin, the protective coating around nerve fibres. This damage disrupts communication between the brain and the body, which leads to neurological symptoms.
Can Stress Trigger MS Symptoms?
Stress does not cause MS, but it can worsen symptoms. Many people with MS notice that high stress levels increase fatigue, muscle tension, or sensory disturbances. Ongoing stress may also contribute to relapse risk in some individuals. Managing stress through sleep, exercise, and psychological support can help stabilise symptoms.
Is There a Blood Test for MS?
There is no single blood test that confirms MS. Doctors use blood tests mainly to rule out other conditions that can mimic MS, such as vitamin deficiencies or infections. Diagnosis relies on MRI scans, neurological examination, and sometimes a lumbar puncture, not on one simple blood result.
When Do MS Symptoms Start?
MS symptoms most commonly begin between ages 20 and 40. However, doctors sometimes diagnose it earlier or later in life. Early symptoms may appear suddenly and include vision changes, numbness, weakness, or unexplained fatigue. Because symptoms vary widely, a neurologist must evaluate persistent or recurring neurological changes.