When people search “CQC Nominated Individual vs Registered Manager”, they want one clear answer: the Registered Manager runs the service day-to-day, and the Nominated Individual supervises how the organisation runs it.
Both roles sit inside the wider framework of what is CQC registration, the legal process that allows a provider and its manager to carry on regulated activities in England.
The Registered Manager leads daily care delivery, staff performance, safeguarding, and quality assurance at the location. The Nominated Individual represents the provider organisation and supervises the management of those regulated activities at a strategic level.
When both roles work clearly and independently, services perform better under inspection and maintain stronger compliance.
If you are:
- Registering a new service → you must understand what registration means for both the provider and the manager.
- Restructuring leadership → you must define authority and oversight clearly.
- Preparing for inspection → you must show how these two roles produce consistent, evidence-backed governance.
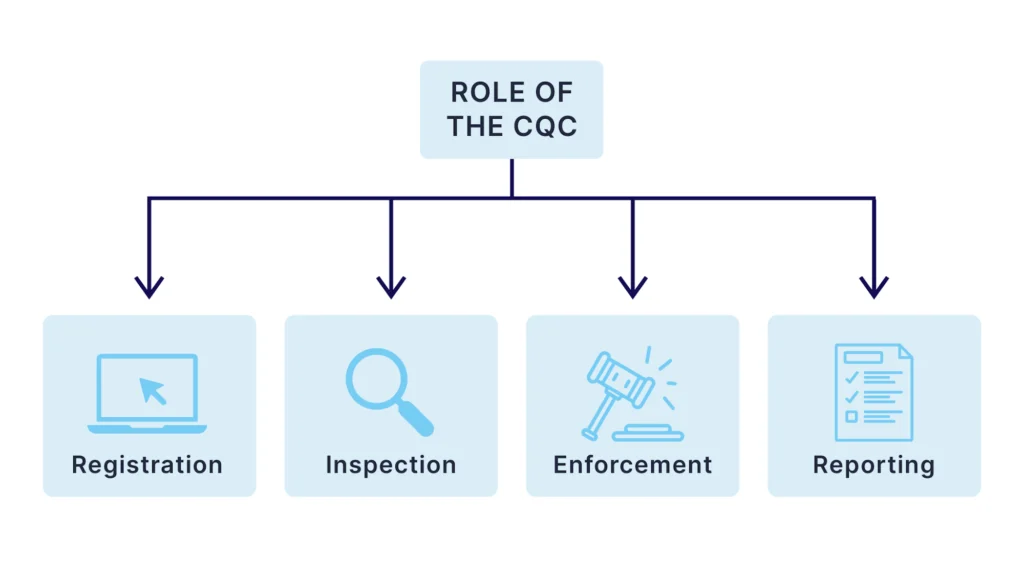
What Does Registration Mean in Care?
Before you compare leadership roles, you must understand what registration means in health and social care.
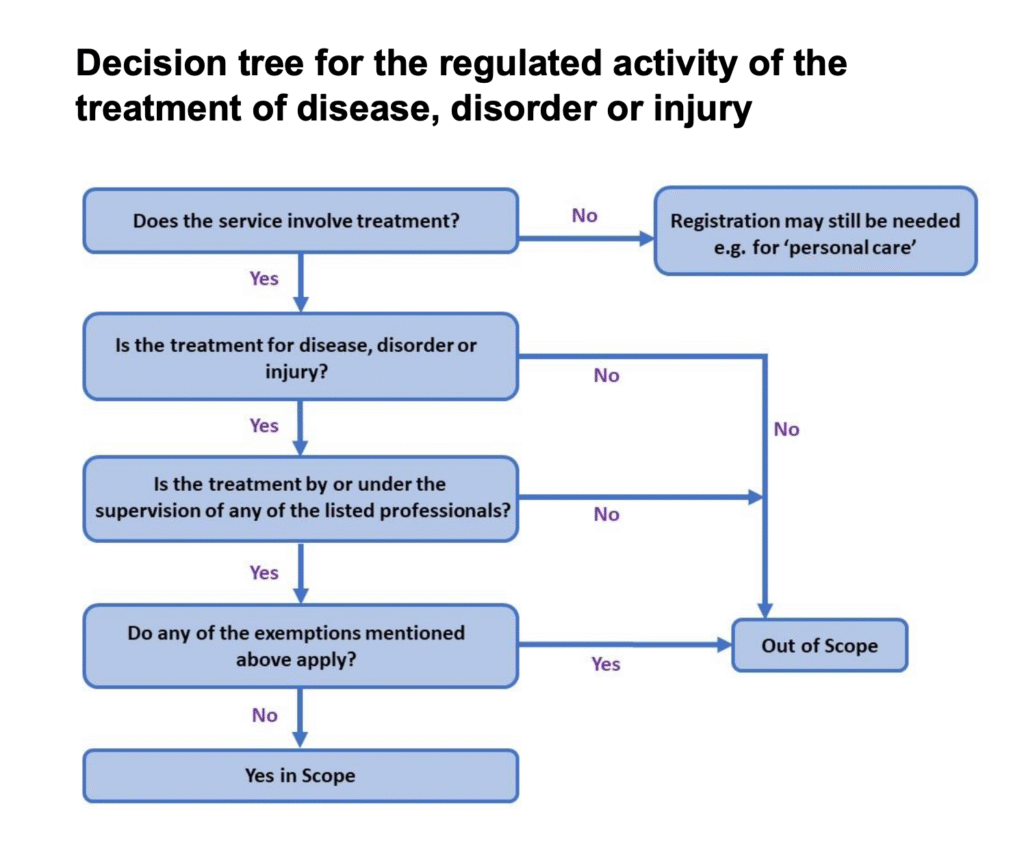
In England, registration is the legal approval granted by the Care Quality Commission (CQC) that allows a provider to carry on regulated activities, such as personal care, treatment of disease, or accommodation with nursing. If you provide regulated activities without registration, you commit a criminal offence.
So when people ask:
- What is registration?
- What are registrations in care?
- What does registration mean?
They are really asking: Who holds legal responsibility for delivering regulated activities safely and lawfully?
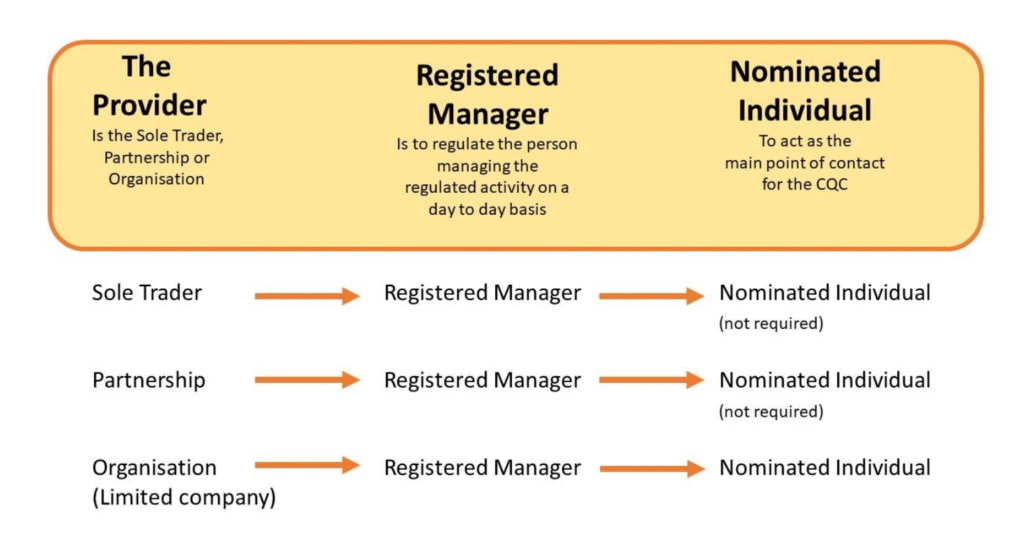
Under CQC law, registration applies to:
- The Provider (the organisation or individual running the service)
- The Registered Manager (the person responsible for managing regulated activities at a location)
The Nominated Individual does not register in the same way as a Registered Manager. Instead, the provider appoints them to supervise the management of regulated activities on behalf of the organisation.
In simple terms:
- Registration creates legal accountability
- It defines who CQC can hold responsible
- It determines who must demonstrate fitness, competence, and good character
Understanding this foundation makes the leadership split between Nominated Individual and Registered Manager much easier to grasp, and much harder to get wrong.
RELATED: CQC Registered Manager: Dismissal and How to Pass the Interview (2026)
CQC Nominated Individual vs Registered Manager: The Difference at a Glance
If you strip away jargon, the difference becomes simple and practical.
When people ask, “What is the role of a nominated individual CQC?”, they want clarity. They want to know who actually runs the service and who holds the bigger picture together.
Here is the clean comparison:
| Area | Registered Manager (RM) | Nominated Individual (NI) |
| Primary Focus | Runs the service day-to-day | Supervises how the service is managed |
| Legal Status | A registered person with CQC | Appointed by the provider (not a registered person) |
| Main Accountability | Daily compliance with regulations at the location | Organisational oversight and governance |
| Typical Responsibilities | Staffing, care quality, safeguarding, audits, incident management | Governance systems, resource allocation, strategic risk, holding the RM accountable |
| CQC Interaction | Main operational contact for inspections and notifications | Senior representative when escalation or strategic oversight is required |
| Common Failure Pattern | Lacks authority to fix problems | Has title but no real governance power |
CQC Nominated Individual Requirements (In Plain English)
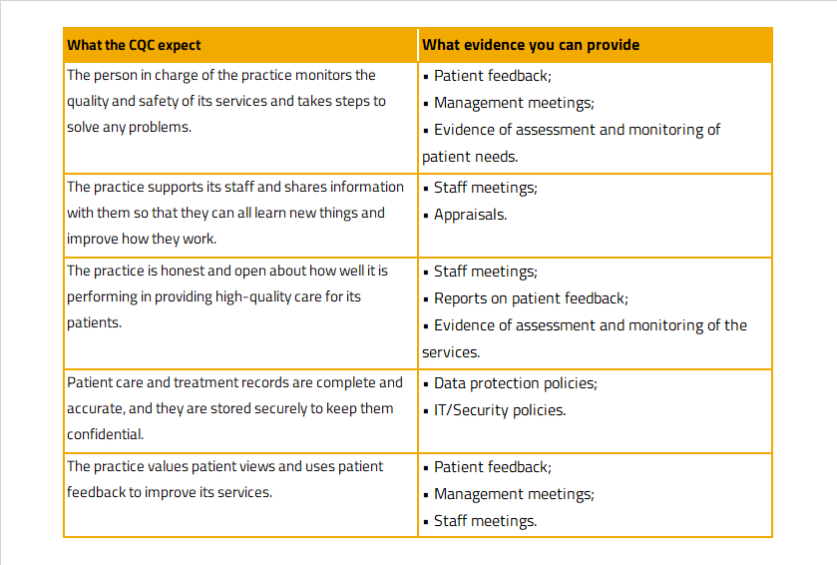
CQC expects the Nominated Individual to:
- Be a director, manager, or secretary of the organisation
- Hold enough seniority to influence strategy and resources
- Supervise the management of regulated activities
- Understand the regulatory framework and governance duties
The Registered Manager, by contrast, must register personally with CQC and prove they are fit to manage the regulated activity.
Here’s the simplest way to think about it:
- The Registered Manager converts regulation into daily practice.
- The Nominated Individual ensures the organisation supports, funds, and governs that practice properly.
When these roles overlap without clear boundaries, services drift. When they work together with defined authority and accountability, inspection outcomes improve.
READ MORE: National Minimum Wage 2026 for Care Providers: Compliance Risks and FWA Enforcement
Registered Manager: What You Actually Own Day-to-Day
The Registered Manager carries operational authority. CQC registers you personally because you control how regulated activities run at the location.
If someone asks how to become a registered manager, the short answer is this: you must demonstrate leadership experience, sector competence, and the ability to manage regulated activities safely every single day. CQC will assess your fitness before approving your registration.
But registration alone does not make you effective. Performance does.
What You Control in Practice
A strong Registered Manager owns:
- Daily service delivery quality across all regulated activities
- Staff deployment and supervision. rotas, competency checks, performance management
- Safeguarding response and incident investigation
- Care planning standards and review cycles
- Medication governance (where applicable)
- Audit programmes and action plans
- CQC notifications and compliance deadlines
- Continuous improvement tracking
You do not “oversee” these areas. You run them.
What Great Looks Like
A high-performing Registered Manager:
- Spots risks before they escalate
- Uses audits to drive change, not just tick boxes
- Supports staff but challenges poor performance
- Links complaints and incidents to measurable improvements
- Keeps documentation inspection-ready at all times
When people search how to become a registered care manager or how to become a care home manager, they often focus only on qualifications. Qualifications matter, but leadership discipline matters more.
You must show that you:
- Understand the regulated activity you manage
- Know safeguarding law and reporting duties
- Use data and supervision to improve outcomes
- Take ownership when something goes wrong
In short, the Registered Manager turns regulation into daily behaviour. Without operational control, compliance becomes theoretical, and CQC sees that quickly.
Nominated Individual: How You Supervise Without Micromanaging
The Nominated Individual does not run the service. You supervise how it is run.
When providers ask, “What is the role of a nominated individual CQC?”, the answer is simple: you represent the organisation and make sure the management of regulated activities meets legal and governance standards.
You do not manage rotas.
You do not complete daily audits.
You do not rewrite care plans.
You ensure the systems, leadership, and resources allow those things to happen properly.
Nominated Individual Job Description (Practical Version)
A strong Nominated Individual job description includes responsibility for:
- Setting and reviewing governance structures
- Monitoring quality dashboards and risk registers
- Ensuring adequate staffing levels and training investment
- Reviewing audit results and challenging weak action plans
- Holding the Registered Manager accountable for performance
- Escalating serious risks to the board or owner
- Representing the organisation during CQC engagement
If the Registered Manager owns operations, the Nominated Individual owns assurance.
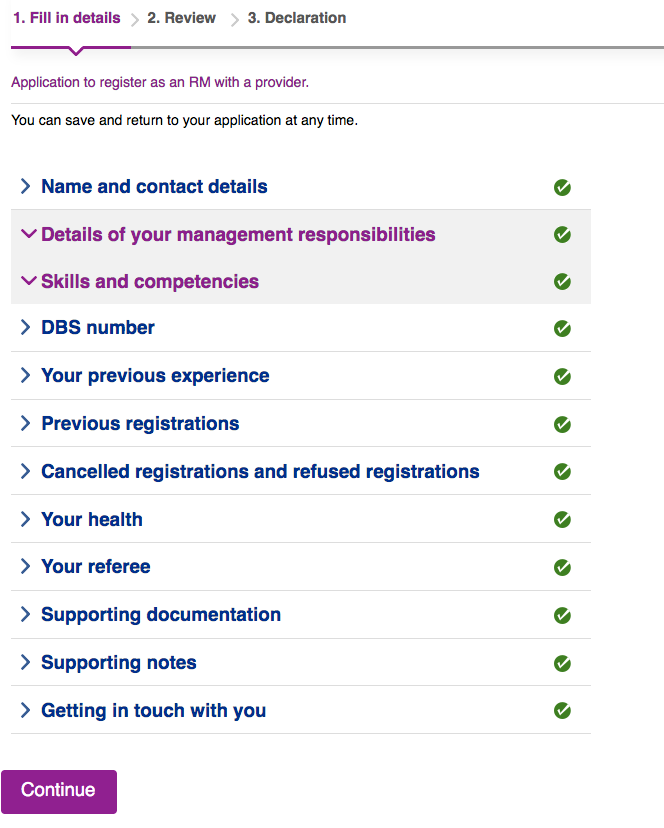
What the CQC Nominated Individual Application Form Tests
The CQC nominated individual application form asks for:
- Your position within the organisation
- Evidence of seniority and authority
- Experience relevant to supervising regulated activities
- Understanding of regulatory duties
CQC does not expect you to run the service yourself. They expect you to understand it well enough to supervise it effectively.
What Strong Governance Looks Like
A high-performing Nominated Individual:
- Reviews monthly quality dashboards and challenges trends
- Demands evidence that action plans close properly
- Ensures the Registered Manager has sufficient authority
- Invests in staffing and training before risk escalates
- Keeps strategic oversight separate from day-to-day operations
Weak NIs create risk when they:
- Hold the title but lack decision-making authority
- Duplicate the RM’s operational work instead of supervising
- Fail to escalate issues beyond the service level
- Ignore early warning signs in audits or complaints
Clear boundaries protect both roles.
The Nominated Individual ensures the organisation has structure, accountability, and resources. The Registered Manager ensures daily care meets standards. When those two functions blur, governance collapses quickly, and CQC notices.
SEE ALSO: Zero Hour Agreement in UK Care: How to Stay Compliant (2026)
Fitness: What “Fit” Actually Looks Like in Practice
CQC does not approve people based on titles. It approves people based on fitness.
When people ask, “What qualifications do I need to be a CQC registered manager?”, they often expect a short answer. The reality requires more than a certificate.
CQC assesses whether you are:
- Of good character
- Competent and experienced
- Healthy enough to perform the role
- Able to provide required documentation
That applies to both the Registered Manager and the Nominated Individual, but the expectations differ.
Registered Manager: Practical Fitness Checklist
To register successfully and perform well, you should have:
- A clear job description defining your authority
- Relevant management experience in a regulated care setting
- A Level 5 Diploma in Leadership and Management for Adult Care (RQF), or clear evidence you are working towards it
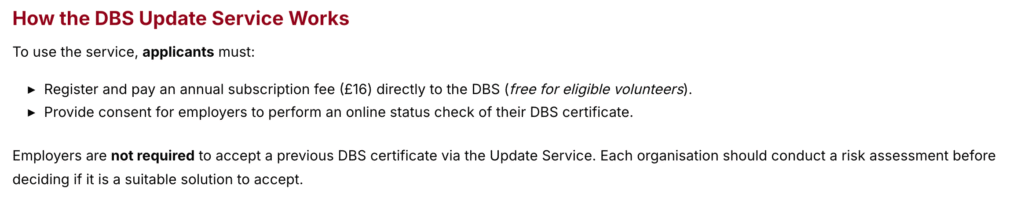
- Enhanced DBS clearance
- A complete employment history with references
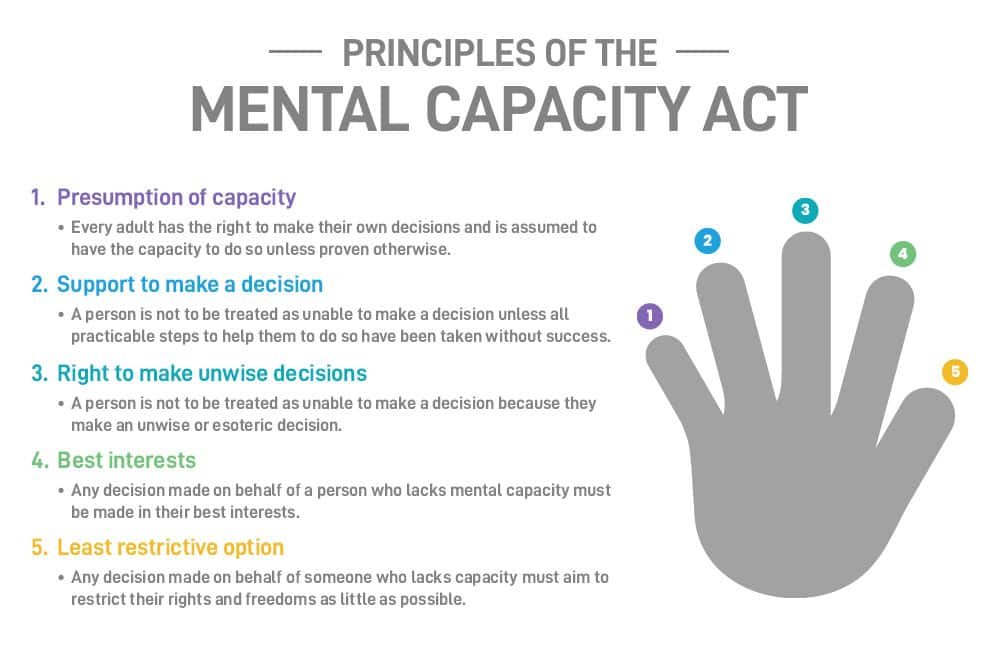
- Strong knowledge of safeguarding, the Mental Capacity Act, and Duty of Candour
- Evidence you can manage audits, complaints, and quality improvement
When people search how to become a manager of a care home, the qualification forms part of the journey, but CQC also expects proven leadership in practice. You must demonstrate that you can manage people, risk, and compliance simultaneously.
Nominated Individual: Practical Fitness Checklist
The CQC nominated individual requirements focus on governance strength, not operational management.
A fit Nominated Individual should demonstrate:
- A senior role within the organisation (director, manager, or secretary)
- Authority to allocate resources and influence strategy
- Clear understanding of the Health and Social Care Act 2008 regulations
- Experience supervising managers or services
- Knowledge of governance systems and risk management
- Ability to hold Registered Managers accountable without undermining them
Fitness, in 2025 and 2026, means more than meeting minimum criteria. It means you can prove, through structure, authority, and competence, that your leadership improves care outcomes.
CQC will test that belief during interview and inspection. If you cannot explain how you lead, challenge, and improve, the registration becomes fragile from day one.
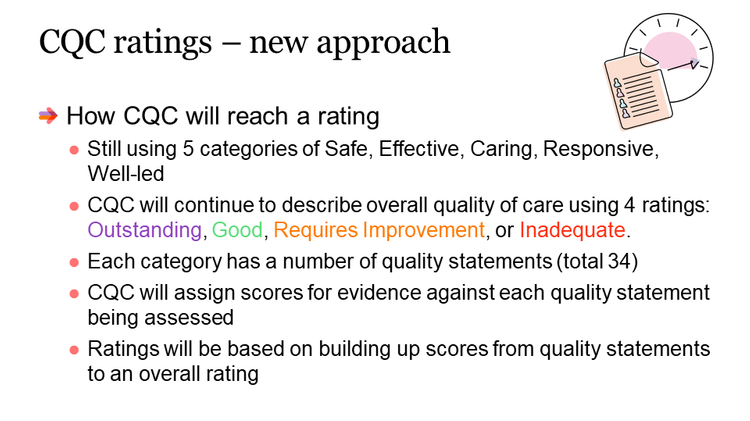
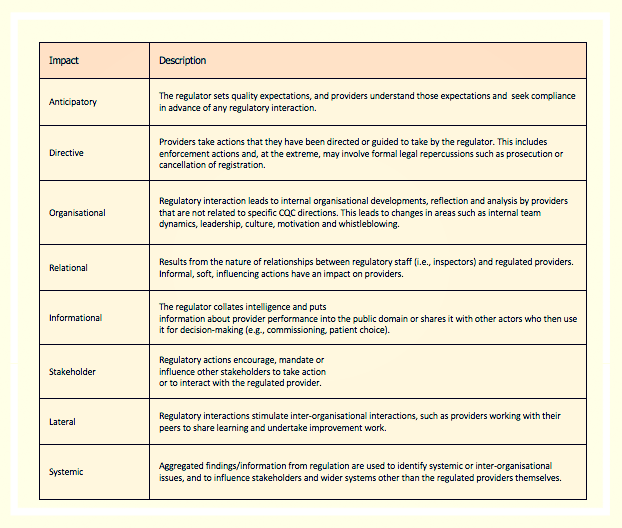
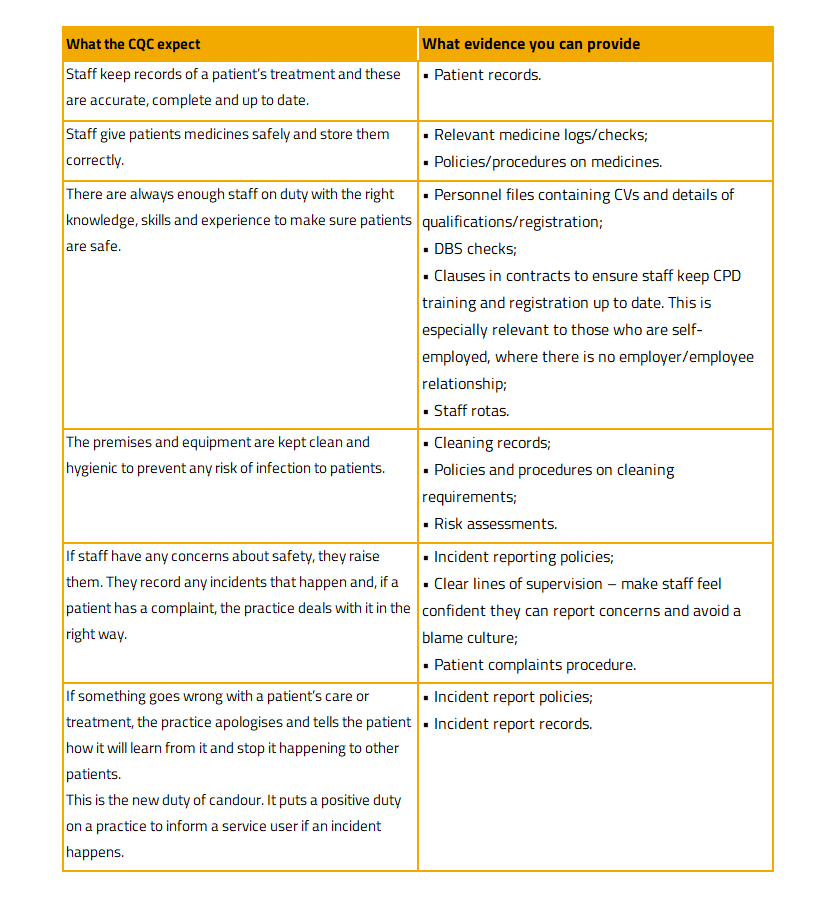
Single Assessment Framework: The 6 Evidence Areas Leaders Must Feed
CQC no longer inspects leadership using the old Key Lines of Enquiry. It now uses the Single Assessment Framework, which gathers evidence continuously across six categories. If you hold either leadership role, you must actively generate evidence in each one.
Inspectors no longer wait for a scheduled visit. They update ratings when evidence changes. That means leadership must produce proof every month, not just before inspection.
Here is how the two roles contribute.
1) People’s Experience
Registered Manager:
- Acts on complaints quickly and shows visible improvements
- Adjusts care plans when needs change
- Protects dignity, safety, and continuity of care
Nominated Individual:
- Reviews complaint themes and trends
- Ensures resources support person-centred care
- Monitors whether improvements stick
2) Feedback from Staff and Leaders
Registered Manager:
- Runs regular supervision and competency reviews
- Resolves staff concerns early
- Builds an open reporting culture
Nominated Individual:
- Reviews staff survey results
- Challenges high turnover or training gaps
- Checks whether supervision leads to action
3) Feedback from Partners
Registered Manager:
- Responds promptly to safeguarding teams and commissioners
- Engages with GPs and professionals
- Documents learning from external concerns
Nominated Individual:
- Reviews partner feedback at governance level
- Escalates recurring themes
- Ensures systemic improvements
4) Observation
Registered Manager:
- Conducts spot checks and care observations
- Reviews medication practice in real time
- Walks the service regularly
Nominated Individual:
- Conducts oversight visits
- Validates audit findings independently
- Checks leadership behaviour on the ground
5) Processes
Registered Manager:
- Maintains audit schedules
- Tracks action plans to completion
- Ensures safe recruitment and notifications
Nominated Individual:
- Reviews governance calendars
- Oversees risk registers
- Monitors whether policies work in practice
6) Outcomes
Registered Manager:
- Reduces missed visits
- Improves medication accuracy
- Improves staff retention and training completion
Nominated Individual:
- Reviews trend data across time
- Allocates resources to correct weak performance
- Ensures improvements sustain
Strong services do not prepare evidence before inspection. They create it weekly through disciplined leadership.
When both roles understand how their work maps to these six evidence areas, inspection stops feeling reactive. Leadership becomes measurable, and that is what CQC now expects.
LEARN MORE: How to Choose Home Care Agencies in the UK (2026)
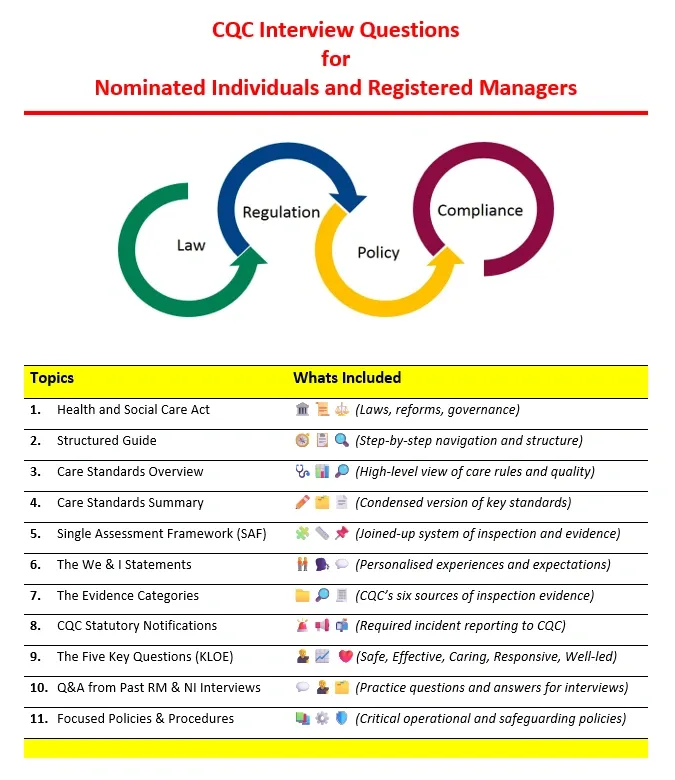
Fit Person Interviews: Questions, Structure, and How to Answer Well
CQC will not approve you on paperwork alone. It will test your understanding, judgement, and leadership through interview.
If you search “Nominated individual CQC interview questions” or “how to become a registered manager”, you usually find vague advice. In reality, CQC interviews focus on how you think, how you act, and how you manage risk.
You must show competence, not memorise regulations.
Registered Manager Interview: What CQC Tests
CQC wants to know whether you can run a regulated service safely every day.
Expect questions like:
1. What are your legal responsibilities as a Registered Manager?
Strong answer structure:
- Reference Regulation 7 and joint accountability with the provider
- Explain daily compliance responsibility
- Mention CQC notifications and safeguarding duties
2. How do you ensure safe care delivery?
Strong answer structure:
- Describe audits, supervision, incident review
- Explain how you identify trends
- Show how you act before risk escalates
3. How would you handle a safeguarding allegation?
Strong answer structure:
- Immediate safety actions
- Reporting to local authority and CQC
- Investigation and learning
- Ongoing monitoring
4. How do you improve a service rated Requires Improvement?
Strong answer structure:
- Assess risk areas first
- Prioritise urgent safety issues
- Build a clear action plan
- Engage staff
- Track measurable outcomes
Nominated Individual Interview: What CQC Tests
CQC wants to see strategic oversight, not operational detail.
Expect questions like:
1. How do you supervise the management of regulated activities?
Strong answer structure:
- Governance meetings
- Quality dashboards
- Risk register oversight
- Clear escalation routes
2. How do you ensure adequate resources?
Strong answer structure:
- Staffing models
- Budget decisions
- Training investment
- Capacity planning
3. How do you hold the Registered Manager accountable?
Strong answer structure:
- Performance reviews
- Governance review meetings
- Evidence-based challenge
- Action tracking
Use the STAR Method for Every Answer
Structure responses clearly:
- Situation – Brief context
- Task – Your responsibility
- Action – What you actually did
- Result – What improved and how you measured it
CQC does not reward theory. It rewards demonstrated impact.
If you cannot explain how your leadership improved safety, compliance, or outcomes, the interview will expose the gap quickly.
ALSO: New Rules for Care Home Payments in 2026
Costs and Salary: What People Actually Want to Know
Leadership roles also raise practical questions about money and commitment. If you plan to register or restructure, you must understand both registration costs and leadership remuneration.
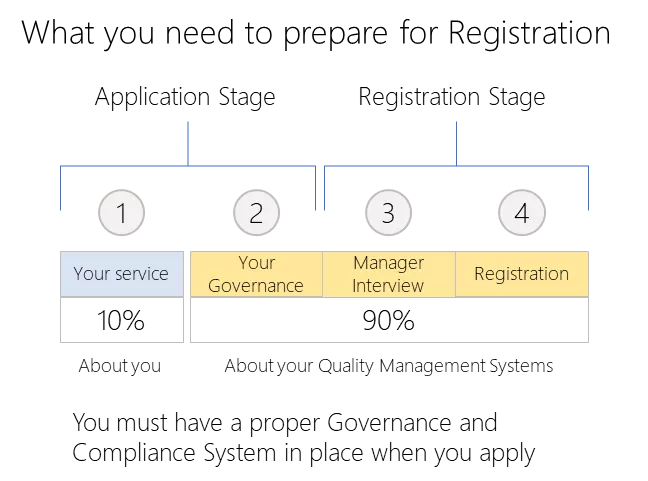
How Much Does CQC Registration Cost?
When people ask, “How much does CQC registration cost?”, the answer depends on the type of regulated activity you provide and the size of your service.
CQC charges:
- An application fee when you first register
- An annual fee based on the type and scale of your regulated activities
For example, a small domiciliary care agency pays less than a large care home group operating multiple locations. CQC publishes an annual fee scheme that sets out the exact bands and rates. You should always check the current fee structure before budgeting.
Registration costs go beyond CQC fees. You should also budget for:
- DBS checks
- Professional indemnity insurance
- Policy development
- Leadership training
- Governance systems
Underestimating these costs often weakens services before they even open.
CQC Nominated Individual Salary
Search interest around “CQC nominated individual salary” continues to grow. Salary varies significantly depending on:
- Organisation size
- Number of locations
- Complexity of regulated activities
- Level of governance responsibility
- Geographic location
In smaller organisations, a director or owner often holds the role without separate pay. In larger providers, especially multi-site operations, the role may form part of a senior executive salary package.
The key principle remains consistent: CQC expects the Nominated Individual to hold genuine authority and accountability. Compensation should reflect that responsibility. Underpaying or under-resourcing this role usually signals weak governance, and weak governance rarely survives inspection pressure.
If you structure leadership correctly from the beginning, costs become investment rather than damage control.
When One Person Holds Both Roles: Risks and Safeguards
In very small organisations, one person may act as both the Registered Manager and the Nominated Individual. CQC allows this arrangement, but it creates governance risks that you must manage carefully.
The problem is simple: one person cannot effectively supervise themselves.
When you combine the roles without safeguards:
- Operational decisions go unchallenged
- Governance becomes reactive
- Escalation routes disappear
- Risk blind spots increase
- Inspection conversations lack independent oversight
CQC expects separation wherever possible because it strengthens accountability. If concerns arise about service management, inspectors need someone senior to challenge and correct the issue. When both roles sit with one person, that escalation becomes weaker.
If You Must Combine the Roles, Do This
If your organisation genuinely cannot separate the roles, implement safeguards immediately:
- Create external oversight. Arrange regular supervision or governance review with an independent consultant, mentor, or board member.
- Separate documentation. Maintain distinct operational records (RM duties) and governance records (NI duties), even if you produce both.
- Formalise escalation routes. Ensure the board or owner receives direct risk reports without filtering.
- Schedule structured governance reviews. Conduct quarterly reviews that focus purely on strategic oversight, not daily management.
- Document the arrangement clearly. Explain to CQC how you prevent self-supervision and how you maintain challenge.
Treat the dual role as two jobs with two mindsets. Switch deliberately between operational execution and strategic oversight.
Strong providers never rely on informal arrangements. They design governance deliberately, even when resources feel tight.
READ: Care Policies and Procedures: How to Implement Them Correctly in 2026
Leadership Evidence Packs: What to Have Ready at All Times
If CQC visited tomorrow, could you produce leadership evidence within minutes?
Strong services do not scramble for documents. They maintain structured evidence folders that reflect daily discipline.
Below are practical, inspection-ready checklists for both roles.
Registered Manager Evidence Folder
Keep this organised and current:
Personal and Registration Records
- Job description with defined authority
- CQC registration certificate
- Level 5 qualification (or proof of working toward it)
- Enhanced DBS certificate
- Employment history and references
- CPD and leadership training records
Operational Governance
- Audit schedule and recent audit results
- Action plan tracker with named owners and deadlines
- Supervision schedule and supervision records
- Training matrix with completion rates
- Safeguarding log with learning outcomes
- Incident log with investigation summaries
- Complaints and compliments log with theme analysis
- CQC notifications submitted (copies retained)
- Monthly quality dashboard with trend commentary
If you ask yourself “how to become a registered manager”, this folder answers the real question: demonstrate structured leadership.
Nominated Individual Evidence Folder
Your folder should show oversight, not operational duplication.
Governance Structure
- Governance calendar (monthly and quarterly cycles)
- Governance meeting minutes with tracked actions
- Strategic risk register
- Provider-level quality reports
Oversight and Accountability
- Evidence of reviewing audit trends
- Records of performance challenge meetings
- Resource allocation decisions and rationale
- Staff survey results and follow-up actions
- Board or owner reporting summaries
Regulatory Engagement
- Records of CQC engagement
- Documentation of strategic improvements
- Evidence of monitoring compliance deadlines
If someone asked you to write a Nominated Individual job description, this evidence pack would define it.
Strong leadership leaves a trail.
If your systems generate evidence naturally through weekly and monthly rhythms, inspection becomes validation, not crisis management.
Now that we’ve mapped the structure, responsibilities, interviews, costs, and evidence, the final step is clarity: avoid the mistakes that cause leadership failures during inspection.
The Mistakes That Damage Leadership, and How to Avoid Them
Most services do not fail inspection because they lack policies. They fail because leadership lacks clarity, authority, or discipline.
If you want to strengthen your position under CQC Nominated Individual vs Registered Manager scrutiny, avoid these common errors.
Mistake 1: The Nominated Individual Has the Title, Not the Power
Some providers appoint a Nominated Individual in name only. The person attends meetings but cannot approve budgets, influence staffing, or challenge poor performance.
CQC expects the Nominated Individual to supervise management meaningfully. If they cannot allocate resources or escalate risks, governance collapses.
Fix:
Appoint someone with genuine senior authority. Give them visibility of financial, staffing, and quality data. Make challenge part of the culture.
Mistake 2: The Registered Manager Has Responsibility, Not Authority
CQC holds the Registered Manager accountable for compliance. Yet some providers restrict their decision-making power.
If the RM cannot:
- Adjust staffing levels
- Enforce training standards
- Escalate safety concerns
- Implement corrective actions
then compliance becomes cosmetic.
Fix:
Define decision boundaries clearly. Document what the RM can decide independently and what requires escalation. Align accountability with authority.
Mistake 3: Governance Happens Only Before Inspection
Some services tighten audits and update documents only when they hear inspection rumours. Under the Single Assessment Framework, that strategy fails.
CQC can update ratings based on ongoing evidence. Weak governance leaves long gaps in documentation and improvement tracking.
Fix:
Implement a weekly and monthly rhythm. Generate evidence continuously. Treat governance as a system, not an event.
Mistake 4: No Clear Split Between Operations and Oversight
When the Nominated Individual starts running the service directly, or the Registered Manager attempts to control strategic governance, confusion follows.
Blurring the line weakens accountability and creates blind spots.
Fix:
Write down the role split. Review it quarterly. Ensure everyone in the organisation understands who leads daily operations and who supervises management.
Mistake 5: Poor Interview Preparation
Some applicants assume experience alone will carry them through the CQC interview. When they cannot explain safeguarding processes, governance structures, or improvement methods clearly, confidence drops.
CQC does not expect perfection. It expects competence and structured thinking.
Fix:
Prepare answers using real examples. Practise explaining how your actions improved outcomes. Use the STAR method consistently.
Mistake 6: Ignoring the Human Side of Leadership
Leadership does not live in dashboards alone. If staff feel unsupported or unable to raise concerns, problems multiply quietly.
Strong services build psychological safety. Weak services silence it.
Fix:
Hold open forums. Review exit interviews. Act on staff feedback visibly. Make challenge safe and routine.
When leadership roles operate clearly and actively, not symbolically, services move from reactive compliance to confident governance.
Final Thoughts…
The difference between a fragile service and a confident one often comes down to this:
- The Registered Manager runs the service with authority and discipline.
- The Nominated Individual supervises management with independence and challenge.
That is the real meaning behind CQC Nominated Individual vs Registered Manager.
When you define the roles clearly:
- Governance produces evidence naturally.
- Interviews feel structured, not stressful.
- Audits drive improvement, not paperwork.
- Staff understand who leads what.
- CQC sees consistency instead of confusion.
When you blur the roles:
- Accountability weakens.
- Risks hide in operational gaps.
- Oversight disappears.
- Inspection outcomes deteriorate.
If you are asking:
- How to become a registered manager
- What qualifications do I need to be a CQC registered manager
- What is the role of a nominated individual CQC
The real answer goes beyond qualifications and titles. It comes down to authority, structure, and disciplined governance.
Strong leadership leaves an evidence trail. Weak leadership leaves explanations.
If you want your leadership setup to feel calm, structured, and inspection-ready, rather than reactive and uncertain, design your roles deliberately. Build rhythm into governance. Generate evidence weekly. Prepare for interviews properly.
CQC does not reward paperwork. It rewards leadership that produces safe, sustainable outcomes.
Ready to Strengthen Your CQC Leadership Structure?
A clearly defined leadership model does more than satisfy CQC regulations. It protects your rating, reduces enforcement risk, and builds commissioner confidence in your service.
Care Sync Experts supports domiciliary care agencies, supported living providers, and care homes across the UK with:
- Full leadership structure reviews aligned with CQC regulations
- Registered Manager fitness and interview preparation
- Nominated Individual governance framework design
- Single Assessment Framework evidence mapping
- Governance calendar and quality dashboard implementation
- Dual-role risk assessments and safeguard design
- Mock inspections focused on the “Well-led” key question
- Evidence pack preparation for inspection and registration
Whether you are registering a new service, restructuring leadership, or preparing for inspection, we help you build systems that stand up to scrutiny and perform consistently under pressure.
Get in touch with Care Sync Experts today to move forward with clarity, authority, and inspection-ready leadership.
FAQ
What does “nominated person” mean?
In the CQC context, a nominated person usually refers to the Nominated Individual appointed by a provider organisation. The provider selects this person to represent the organisation and supervise the management of regulated activities.
Outside CQC language, “nominated person” can simply mean someone chosen for a specific responsibility. Under CQC regulation, however, it has a defined governance meaning: the person must supervise how regulated activities are managed and ensure the organisation meets legal standards.
Is a nominated individual the same as a registered manager?
No. A Nominated Individual is not the same as a Registered Manager.
The Registered Manager runs the service day-to-day and registers personally with CQC. The Nominated Individual represents the provider organisation and supervises how the service is managed.
The Registered Manager holds operational responsibility.
The Nominated Individual holds governance oversight responsibility.
CQC expects clear separation between these functions wherever possible.
What are the different CQC ratings?
CQC uses four ratings to judge services:
Outstanding – The service performs exceptionally well.
Good – The service meets standards consistently and delivers safe, effective care.
Requires Improvement – The service does not consistently meet standards and must improve.
Inadequate – The service fails to meet required standards and may face enforcement action.
CQC applies these ratings across five key questions: Safe, Effective, Caring, Responsive, and Well-led. Leadership quality strongly influences the Well-led rating.
What is the lowest CQC rating?
The lowest CQC rating is Inadequate.
When CQC rates a service Inadequate, it has identified serious failings in safety, leadership, or care quality.
CQC may impose conditions, restrict admissions, issue warning notices, or begin enforcement action. In some cases, services close if they cannot improve.
Leadership failures often contribute to an Inadequate rating, particularly under the Well-led key question.