Sometimes, but the trigger is personal care, not supported living itself. The Care Quality Commission (CQC) does not regulate supported living as a service model. CQC only regulates what you do inside that model.
If your staff deliver personal care, you must register with CQC before you start operating. If you do not provide personal care, CQC registration is not required.
What counts as personal care?
CQC defines personal care as hands-on support with daily living tasks, including:
- Washing or bathing
- Dressing or undressing
- Toileting or continence care
- Eating or drinking support
- Physical assistance linked to hygiene or mobility
If your staff help with any of these activities, even occasionally, you are delivering the regulated activity of personal care. You need CQC registration before providing these services.
What does not trigger CQC registration?
You do not need CQC registration if your service only provides housing-related or social support, such as:
- Tenancy sustainment
- Budgeting or bill support
- Help accessing education, work, or community activities
- Emotional or social support without hands-on care
Many supported living providers fall into this category at first. Problems arise when services quietly drift into personal care without recognising the regulatory consequences.
CQC treats unregistered personal care as a serious offence. Operating without registration can lead to enforcement action, prosecution, and long-term reputational damage.
Just as importantly, CQC does not accept “grey areas.” If inspectors see evidence of personal care, they will assess your service against the standards for regulated activity, regardless of how you describe your model.
Supported living does not require CQC registration by default. Personal care does. If your service crosses that line, registration is mandatory, and getting it wrong can cost you months of delays or force a complete reapplication.
CQC Supported Living vs Care Homes
Many providers lose registrations or face reclassification because they misunderstand this distinction. CQC does not judge your service by its name. It looks at how you combine housing and care in practice.
The question CQC asks is simple: Does the person genuinely live in their own home, or does the service package accommodation and care together?
What makes supported living legally different from care homes
In supported living, housing and care stay separate.
- The person holds a real tenancy or occupancy agreement
- Housing and care sit under separate legal arrangements
- The tenant can, in principle, change their care provider without losing their home
- Staff respect the home as the person’s private space, not a service-controlled environment
CQC focuses on choice, control, and housing rights. When those elements exist, the model fits supported living or supported accommodation.
In contrast, care homes operate differently:
- Accommodation and personal care come as a single package
- The provider controls where the person lives and how care is delivered
- Residents do not hold genuine tenancy rights
This difference explains why someone searching for care homes near me looks for a regulated residential setting, while supported living operates under a completely different legal framework.
When supported living becomes an assisted care facility
Problems arise when providers blur the line.
CQC may decide your service functions as an assisted care facility or care home if it sees evidence that:
- Care is tied to the property
- Tenants cannot realistically choose or change their care provider
- Staff access the home without proper consent or boundaries
- Commissioners “place” people into a bundled housing-and-care arrangement
- The service controls daily living decisions rather than supporting independence
When this happens, CQC may conclude that you are providing accommodation together with personal care. That triggers a different regulated activity, with higher expectations, different registration requirements, and stricter inspection standards.
CQC makes this judgement based on evidence, not intent. Even well-meaning providers fail here because their documents, contracts, or daily practice contradict the supported living model they describe.
Why getting this wrong causes serious problems
If CQC determines that your service operates like a care home:
- Your CQC Supported Living application may fail
- You may need to reapply under the correct regulated activity
- Your registration timeline can extend by months
- Future inspections will assess you against the wrong framework
In extreme cases, CQC can refuse registration altogether if it believes the model does not protect people’s rights or independence.
Supported living succeeds only when housing and care remain genuinely separate. If accommodation and care merge into a single package, CQC will treat the service as something else entirely, regardless of what you call it.
The Real Tenancy Test: How CQC Decides If Your Model Is Genuine
This is where most CQC Supported Living applications succeed or fail. CQC does not rely on labels like supported living or supported accommodation. It looks for evidence that people genuinely live in their own homes.
To make that judgement, the Care Quality Commission refers to the Real Tenancy Test, a framework developed by the National Development Team for Inclusion (NDTi) and embedded in CQC’s Housing with Care guidance.
CQC uses this test to answer one question: Does the person have real housing rights and real control over their home?
What the Real Tenancy Test actually checks
CQC expects supported living providers to show that housing and care operate as two genuinely separate arrangements, not a bundled service.
Key indicators of a genuine supported living model include:
- The person holds a legal tenancy or occupancy agreement with enforceable housing rights
- Housing and care sit under separate contracts, not a single package
- The care provider and housing provider are separate organisations, or clearly separated functions if part of the same group
- The tenant can choose or change their care provider without losing their home
- Staff treat the property as the person’s private home, not a service location
- The tenant controls access, routines, and decisions about their living space
- Commissioners do not “place” people into a fixed housing-and-care bundle
CQC looks for consistency across documents, contracts, and daily practice. If any part of your model contradicts these principles, assessors will question whether your service truly qualifies as supported living.
Common ways providers fail the Real Tenancy Test
Many applications fail not because providers misunderstand the law, but because their evidence tells a different story.
CQC often raises concerns when it sees:
- Care contracts that reference the property as a “placement”
- Housing agreements that end automatically if care stops
- Staff holding keys without tenant consent or clear access protocols
- Service rules that override tenant choice “for operational reasons”
- Care rotas that dictate daily life rather than support independence
Each of these signals suggests that accommodation and care operate as one service. When that happens, CQC may decide the model no longer fits supported living.
Why the Real Tenancy Test affects your registration outcome
If your service fails the Real Tenancy Test, CQC may conclude that you provide accommodation together with personal care. That triggers a different regulated activity and a completely different registration route.
This decision can lead to:
- Rejection of your supported living application
- Requirement to reapply under a care home-style registration
- Significant delays and added costs
- Higher inspection thresholds and tighter regulatory scrutiny
CQC makes this decision early in the process. Once assessors form the view that housing and care are not genuinely separate, reversing that conclusion becomes difficult.
Passing the Real Tenancy Test is not about wording. It depends on how your service works in reality. If tenants hold real housing rights and real control, CQC will treat your model as supported living. If not, CQC will regulate it as something else.
READ ALSO: CQC Registration for Domiciliary Care Providers: Complete 2026 Guide
What Changed in CQC Supported Living Registration Since 2025

CQC registration rules for supported living have not stood still. Several changes between 2025 and 2026 have altered how CQC assesses applications, what documents it expects, and how quickly it rejects incomplete submissions.
Understanding these changes helps you avoid costly mistakes.
July 2025 changes: what changed and what did not
In July 2025, the Care Quality Commission introduced a revised registration process aimed mainly at domiciliary care (homecare) providers. Many people assumed those changes applied to supported living. That assumption causes problems.
Here is the reality:
- CQC simplified homecare registration requirements
- Some documents were removed at application stage for homecare only
- CQC tightened rejection rules for incomplete applications
What did not change:
Supported living registration did not receive the same simplifications.
CQC continues to treat supported living as a higher-risk, more complex service model because it sits at the intersection of housing, care, and human rights. As a result, supported living applications still require a broader evidence pack than standard domiciliary care.
February 2026 update: additional supporting documents
In early 2026, CQC expanded the list of supporting documents required for care homes and supported living services.
This update reinforced three key expectations:
- Documents must be current, complete, and service-specific
- Policies must reflect how your service actually operates
- Evidence must align across your Statement of Purpose, business plan, and contracts
CQC now rejects applications more quickly if documents are missing, outdated, contradictory, or clearly copied from generic templates.
This change affects supported living providers more than homecare providers because supported living relies heavily on model clarity. Any inconsistency around housing, care separation, or tenant rights raises immediate concerns.
A critical misconception to avoid
Some providers believe they can submit a “basic” application first and fill in gaps later.
That approach no longer works.
CQC now applies strict initial checks. If your application fails at that stage, CQC rejects it outright. You must correct the issues and resubmit as a new application, losing your place in the queue and adding weeks or months to your timeline.
This is why preparation matters more than speed.
What this means for supported living providers in 2026
If you are registering a supported living service now:
- Do not rely on outdated advice meant for homecare providers
- Assume CQC will scrutinise housing and care separation closely
- Expect rejection if your documents do not align perfectly
- Treat registration as a one-shot submission, not a draft
The registration process has become stricter, not simpler, for supported living. Providers who understand the post-2025 and 2026 changes submit stronger applications, avoid rejection, and move through the process faster.
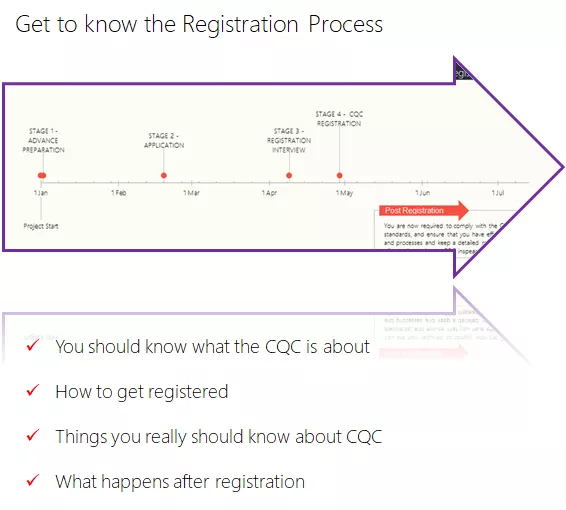
Step-by-Step CQC Supported Living Registration Process
CQC does not approve supported living services by accident. It follows a structured assessment process designed to test whether your organisation can deliver safe, lawful personal care within a genuine supported living model.
Understanding how this process works helps you prepare properly and avoid rejection.
Stage One: Initial checks (the rejection stage)
At this stage, the Care Quality Commission checks whether your application is complete and coherent. CQC does not assess quality here. It checks whether your submission meets the minimum standard to move forward.
CQC will reject your application at this stage if:
- Mandatory forms are missing or incomplete
- Required supporting documents are not attached
- Policies contradict your Statement of Purpose
- Your model of care is unclear or inconsistent
- Housing and care separation is not evident
A rejection at this point means you must resubmit as a new application. You lose your place in the queue and add weeks or months to your timeline.
This is why supported living providers must treat submission as a final version, not a draft.
Stage Two: Full assessment
If your application passes initial checks, CQC moves to full assessment. This is where CQC tests whether you can actually deliver the regulated activity of personal care safely and lawfully.
CQC will assess:
- Your policies and procedures in detail
- Your understanding of supported living principles
- Your leadership and governance arrangements
- Your approach to safeguarding, medicines, and consent
For supported living services, CQC may also arrange a site visit. Inspectors use this to assess premises readiness, privacy, staff access arrangements, and whether the environment supports independence.
The fit person interview
During full assessment, CQC interviews your Registered Manager and Nominated Individual. This interview tests whether the people leading the service meet legal “fit person” requirements.
Expect questions linked to CQC’s five key areas:
- Safe: How you manage safeguarding, risk, and medicines
- Effective: How you deliver person-centred personal care
- Caring: How you protect dignity, privacy, and respect
- Responsive: How you adapt care to individual needs
- Well-led: How you monitor quality and improve practice
For CQC Supported Living, assessors also focus heavily on:
- How you maintain separation between housing and care
- How tenants exercise choice and control
- How staff respect the home as a private space
- How you apply the Mental Capacity Act in daily practice
Weak answers here often lead to delays or refusal.
How long the process takes in practice
CQC aims to process applications within 10 weeks, but supported living registrations often take 10–16 weeks or longer, even for complete applications.
Incomplete or inconsistent submissions extend this timeline significantly. Rejected applications reset the clock entirely.
What happens after registration
Once CQC grants registration:
- You receive your registration certificate
- You can legally begin delivering personal care
- Your service becomes eligible for inspection and future CQC reports
- Your performance will later contribute to published CQC ratings
Registration is not the end of scrutiny. It is the starting point.
CQC registration follows a strict two-stage process. Supported living providers succeed when they submit a complete, consistent application and prepare their leadership team to demonstrate real understanding of supported living, not just paperwork compliance.
MORE: Latest CQC Reports, Regulated Activities (2026)
Documents You Must Submit for CQC Supported Living Registration
CQC expects a complete, consistent evidence pack for supported living registration. Every document must align with your service model and clearly show how you deliver personal care while keeping housing and care separate.
If your documents contradict each other, CQC will reject the application at initial checks.
Core application forms (submit together)
You must submit both provider and manager applications at the same time. CQC will not assess one without the other.
- Application for Registration as a Provider of Regulated Activities
- Application for Registration as a Manager of Regulated Activities
Download the current versions directly from the Care Quality Commission website before completing them. CQC updates forms regularly, and using outdated versions delays assessment.
Statement of Purpose (legal requirement)
Your Statement of Purpose carries legal weight. CQC uses it as the anchor document for the entire application.
For CQC Supported Living, it must clearly state:
- You register for personal care only
- You do not provide accommodation with care
- How housing and care remain separate
- Who you support and how you support them
- Where and how the service operates
- Who manages the regulated activity
CQC frequently rejects applications where the Statement of Purpose sounds like a care home description or fails to explain separation properly.
Mandatory policies and procedures
CQC expects policies that reflect how your service actually works, not generic templates.
At a minimum, include:
- Safeguarding policy and procedures
- Medicines management policy
- Infection prevention and control policy
- Recruitment and safer employment policy
- Consent and Mental Capacity Act policy
- Equality, diversity, and human rights policy
- Complaints policy
- Good governance and quality assurance policy
Each policy must match your client group, staffing model, and supported living approach.
Financial viability statement
Unlike simplified homecare registration, supported living providers must still submit a financial viability statement.
Use the CQC template and include:
- Confirmation of funding sources
- Evidence you can sustain the service as described
- Accountant or financial adviser details
CQC checks whether your financial plan supports safe, continuous care delivery.
Business plan
Your business plan should demonstrate real understanding, not ambition.
CQC looks for:
- Evidence of local need and demand
- Understanding of the people you will support
- Staffing structure and shift patterns
- Risk management and business continuity
- Realistic financial projections
Plans that read like funding pitches often fail this test.
Insurance documentation
You must show evidence of appropriate insurance cover:
- Public liability insurance
- Employer’s liability insurance (if you employ staff)
- Professional indemnity insurance (strongly recommended)
Certificates must show the correct business name and address and remain valid at the time of submission.
Data protection and ICO registration
Even where CQC does not request the certificate at application stage, ICO registration remains mandatory before you process personal data.
CQC may still ask for evidence later in assessment or inspection.
Additional documents CQC often requests later
Prepare these in advance to avoid delays:
- Sample care plan
- Sample care contract (separate from housing agreement)
- Organisational structure chart
- Staff training matrix
- Mental Capacity Act guidance and tools
- Learning Disability form (if applicable)
Why consistency matters more than volume
CQC does not reward long document lists. It looks for alignment.
If your policies describe a service that looks different from your Statement of Purpose, business plan, or contracts, assessors will question whether you understand your own model.
A strong supported living application uses fewer documents, written clearly, that all tell the same story. Consistency across documents is what moves applications forward.
SEE ALSO: New Rules for Care Home Payments in 2026
Personal Care, Medicines, and Mental Capacity in Supported Living
This section causes the most confusion and the most enforcement risk. CQC focuses on what staff actually do, not how providers describe their service.
When personal care triggers CQC registration
Personal care remains the legal trigger. If staff provide hands-on assistance with daily living, registration applies.
That includes:
- Washing, bathing, or personal hygiene
- Dressing or undressing
- Toileting or continence support
- Physical help with eating or drinking
- Direct assistance linked to mobility or hygiene
If your team delivers any of these activities, these services fall within the regulated activity of personal care. You must register before you operate.
Medicines support: the decision rule CQC applies
Medication support creates confusion because not all medicines activity looks the same.
CQC draws a practical line:
- Prompting someone to take their own medicine may not, on its own, trigger registration
- Administering medicines, managing dosages, handling PRN medication, or dealing with medication errors usually sits alongside personal care
When medicines support forms part of a wider personal care role, CQC treats it as ancillary to personal care. In supported living, that often means registration applies even if medicines are not the primary service.
Providers get into trouble when they describe medicines support as “minor” while policies and care plans show otherwise.
Mental Capacity Act: supported living expectations
Supported living providers must show strong, working knowledge of the Mental Capacity Act 2005. CQC looks for evidence that staff:
- Assume capacity unless proven otherwise
- Support people to make their own decisions
- Assess capacity decision by decision
- Record best-interest decisions clearly
- Use the least restrictive options at all times
In supported living, deprivation of liberty works differently from care homes. If a person experiences continuous supervision and control and is not free to leave, providers must seek Court of Protection authorisation. DoLS does not apply.
CQC tests whether managers understand this distinction and apply it correctly in practice.
Consent, choice, and daily living
Supported living succeeds when people control their lives. CQC expects providers to show how they:
- Obtain and record valid consent
- Respect tenancy rights
- Balance safety with independence
- Reduce restrictions over time
Policies alone do not convince assessors. CQC looks for real examples of how staff support people to make choices, even when those choices involve managed risk.
Where providers go wrong
CQC raises concerns when it sees:
- Blanket restrictions “for safety”
- Capacity assessments copied across individuals
- Medication practices that contradict care plans
- Staff uncertainty about when court authorisation applies
When those services drift into risk-averse or institutional practice, CQC questions whether the model still supports independence.
In supported living, personal care, medicines, and mental capacity link together. Providers who understand these links and apply them consistently pass assessment. Those who treat them as paperwork exercises struggle.
LEARN MORE: What does CQC stand for? Complete 2026 Guide
Right Support, Right Care, Right Culture: Requirements for Learning Disability and Autism Services
If your CQC Supported Living service supports autistic people or people with a learning disability, CQC applies additional scrutiny. This is not optional. It is a core part of how the Care Quality Commission decides whether to grant registration.
CQC expects providers to design services around the statutory guidance Right Support, Right Care, Right Culture.
When this guidance applies
CQC applies this framework when your service:
- Supports people with a learning disability
- Supports autistic people
- Offers long-term supported living rather than short-term enablement
If your Statement of Purpose includes these groups, CQC will assess your application against this guidance from day one.
What CQC means by Right Support
Right Support focuses on how the service model promotes independence.
CQC expects you to show that:
- People live in ordinary homes in the community
- Support increases independence rather than replacing it
- Daily routines reflect the person’s choices, not staff convenience
- The service avoids institutional features or restrictive practices
Large, clustered, or highly controlled settings raise red flags unless you provide strong justification.
What CQC means by Right Care
Right Care focuses on how care is delivered.
CQC looks for evidence that care:
- Respects dignity, privacy, and human rights
- Responds to individual needs, not labels
- Supports people to live ordinary lives
- Adapts as people’s needs and goals change
Generic care plans or one-size-fits-all approaches undermine confidence in your model.
What CQC means by Right Culture
Right Culture focuses on leadership and staff behaviour.
CQC expects leaders to create a culture where:
- Staff empower people instead of controlling them
- Risk management supports choice rather than avoids responsibility
- Staff understand autism and learning disability needs
- Managers challenge restrictive or institutional thinking
Culture shows through staff decisions, not policy wording.
Pre-application engagement: when CQC expects it
CQC strongly encourages providers planning learning disability or autism services to engage before submitting a full application.
This usually involves:
- Completing a pre-registration questionnaire
- Discussing your service design with a CQC registration specialist
- Receiving feedback on whether your model aligns with the guidance
Early engagement helps providers avoid rejection after investing time and money in a full application.
Service size and design expectations
CQC often refers to best-practice guidance that supports small, community-based services. There is no absolute size limit, but providers must show that:
- The environment supports privacy and dignity
- Staffing levels remain appropriate
- The setting does not feel institutional
CQC has refused registrations where providers failed to show how service design supports person-centred care. It has also approved larger services where providers demonstrated strong evidence of individualised support.
Training expectations and the Oliver McGowan Code
CQC expects providers to train staff appropriately for the people they support.
For learning disability and autism services, this includes meeting the standards set out in the Oliver McGowan Mandatory Training Code of Practice. CQC checks whether:
- Staff receive training relevant to their role
- Training supports real competence, not box-ticking
- Supervision reinforces good practice
Training records must match your staffing model and service aims.
Why this section matters for registration
CQC uses Right Support, Right Care, Right Culture as a registration filter, not just an inspection framework. If your service design conflicts with this guidance, CQC may refuse registration even if your paperwork looks complete.
For learning disability and autism services, CQC does not ask whether you can deliver care. It asks whether your service model supports people to live ordinary, empowered lives. Providers who design around this principle move forward. Those who ignore it get stopped early.
ALSO READ: Care Policies and Procedures: How to Implement Them Correctly in 2026
The Fit Person Interview: How CQC Assesses Your Leadership
CQC does not register services. It registers people. The fit person interview decides whether your leadership team is capable of running a supported living service safely, lawfully, and in line with regulatory expectations.
This interview often determines the outcome of the application.
Who CQC interviews and why
The Care Quality Commission interviews:
- The Registered Manager
- The Nominated Individual (if applicable)
CQC uses the interview to confirm that these individuals:
- Are of good character
- Can perform the duties of their role
- Have the skills, knowledge, and experience to manage personal care in supported living
Strong paperwork cannot compensate for weak leadership responses.
How CQC structures the interview
CQC frames the interview around its five key questions. Assessors expect clear, confident, and practical answers.
Safe
You must explain how you:
- Identify and manage safeguarding risks
- Respond to incidents and near misses
- Handle medicines safely
- Protect people from avoidable harm
Expect scenario-based questions, not theory.
Effective
CQC tests whether you:
- Deliver person-centred personal care
- Apply Mental Capacity Act principles correctly
- Assess capacity decision by decision
- Review care as needs change
Generic answers raise concerns.
Caring
You need to show how you:
- Promote dignity, privacy, and respect
- Support people to make real choices
- Avoid institutional practices
- Balance risk with independence
CQC looks for values in action, not slogans.
Responsive
CQC wants to know how you:
- Adapt support to individual needs
- Respond to complaints
- Learn from feedback
- Adjust care quickly when circumstances change
Rigid systems signal poor responsiveness.
Well-led
This is where many providers struggle.
You must explain how you:
- Monitor quality and performance
- Audit care delivery
- Learn from incidents and inspections
- Lead staff culture and behaviour
Good governance matters more than policy volume.
Supported living–specific questions to expect
For CQC Supported Living, assessors focus heavily on:
- How you maintain separation between housing and care
- How tenants control access to their home
- How staff respect tenancy rights
- How you apply the Real Tenancy Test in daily practice
- How you reduce restrictions over time
If leaders cannot explain these clearly, CQC questions whether the model truly supports independence.
What weak interviews have in common
CQC often raises concerns when interviewees:
- Rely on policy wording instead of real examples
- Confuse supported living with care home practice
- Show uncertainty around mental capacity or court authorisation
- Cannot explain how governance works in practice
Experience matters here. Leaders familiar with regulatory environments, whether through management roles, inspection experience, or regulatory careers such as CQC careers or care quality commission jobs, tend to perform better because they understand how assessors think.
How to prepare effectively
Strong preparation focuses on real scenarios, not memorised answers.
Before the interview, ensure you can explain:
- How your service works on a typical day
- How staff make decisions when risks arise
- How you evidence learning and improvement
- How leadership supports independence, not control
Practice answering questions out loud. If you cannot explain something simply, CQC will assume the system is not embedded.
CQC uses the fit person interview to test leadership credibility. Providers who demonstrate clarity, confidence, and real understanding of supported living principles move forward. Those who rely on paperwork alone often do not.
Anti-Rejection Checklist: How to Avoid Common CQC Registration Failures
Most CQC Supported Living applications do not fail because providers lack good intentions. They fail because documents, decisions, and service design do not line up.
Use this checklist before submission. Treat it as a final gate, not a formality.
Documentation consistency (non-negotiable)
CQC cross-checks every document you submit. Inconsistencies trigger immediate rejection.
Confirm that:
- Your Statement of Purpose matches your policies, staffing model, and client group
- Your business plan describes the same service as your policies
- Housing and care separation appears clearly across all documents
- Organisational charts match named roles elsewhere
- Every document uses the same legal business name
If one document describes a care-home-style service, CQC will assume that is your true model.
Completeness of submission
CQC now rejects incomplete applications at initial checks.
Before sending anything, confirm that:
- All mandatory policies are attached
- All required forms are completed in full
- All signatures are included
- Insurance certificates are current and accurate
- Files are readable and clearly named
- Everything is submitted together in one package
Sending documents in stages does not help. It delays or resets your application.
Supported living-specific checks
This is where many providers fail.
Confirm that you can clearly evidence:
- Genuine separation between housing and care
- A real tenancy or occupancy agreement
- A care contract separate from housing
- Tenant control over access, routines, and decisions
- Compliance with the Real Tenancy Test
If you cannot demonstrate this, CQC may treat your service as a care home and reject the application.
Learning disability and autism services
If your service supports autistic people or people with learning disabilities, check that:
- Your service design aligns with Right Support, Right Care, Right Culture
- You have evidence of commissioner engagement
- You completed pre-application discussions where expected
- Staff training plans meet current guidance
CQC rejects services that appear institutional, restrictive, or poorly designed for independence.
Regulatory currency
Outdated information causes rejection.
Before submission:
- Download the latest forms from the CQC website
- Review current guidance and supporting document requirements
- Update policies to reflect current legislation
- Remove any references to outdated processes or systems
CQC does not correct outdated submissions. It rejects them.
Final self-test before submission
Ask yourself these questions honestly:
- Would an assessor understand our service model in five minutes?
- Do all documents tell the same story?
- Can our leaders explain this model confidently in interview?
- Does our service protect tenancy rights and independence?
If the answer to any question is no, stop and fix the issue before submitting.
CQC rejection usually signals misalignment, not malice. Providers who submit a clear, consistent, supported living model move forward. Those who rush or rely on generic documents get stopped early.
CQC Fees, Timelines, and What Happens After You Register
Registering a supported living service involves more than approval paperwork. Providers need to understand costs, realistic timelines, and post-registration expectations to plan properly and avoid disruption.
CQC fees for supported living providers
There is no application fee for CQC registration. However, once registration is granted, providers must pay an annual fee.
For community social care providers, which includes CQC Supported Living, CQC calculates fees using:
- A base fee
- A per–service user fee
The exact amount depends on how many people you support. Fees are invoiced after registration and then annually. Providers must budget for this from day one, as non-payment creates compliance risks.
How long registration takes in practice
CQC’s official target remains 10 weeks, but supported living registrations often take 10 to 16 weeks or longer.
Timelines depend on:
- Completeness of your application
- Clarity of your supported living model
- Speed of responses to CQC queries
- Interview availability for key personnel
Rejected applications restart the clock entirely. This is why preparation saves months.
What happens immediately after registration
Once CQC grants registration:
- You receive your registration certificate
- You can legally deliver personal care
- Your service becomes eligible for inspection
- CQC can publish a CQC report after inspection
Registration does not mean reduced scrutiny. It signals that CQC expects you to operate exactly as described.
Inspections, reports, and ratings
CQC will usually inspect supported living services within the first year. Inspectors assess whether your service remains:
- Safe
- Effective
- Caring
- Responsive
- Well-led
Inspection outcomes feed into published CQC ratings, which commissioners and families rely on heavily.
Strong early practice helps you avoid adverse CQC reports that can affect referrals and funding.
Why inspection readiness matters from day one
CQC inspects against real practice, not application promises.
Inspectors will review:
- Care delivery
- Record keeping
- Staff competence
- Tenant rights and privacy
- Leadership and governance
Providers who drift from their registered model often struggle at first inspection.
How registration affects commissioning and growth
A strong registration and inspection history helps supported living providers:
- Secure local authority referrals
- Build credibility within Care United Kingdom and the wider sector
- Compete with large providers such as Barchester Care Home groups
- Demonstrate compliance when bidding for contracts
Poor inspection outcomes, by contrast, limit growth opportunities.
Registration opens the door, but inspection determines reputation. Providers who plan for compliance beyond registration build stronger, more sustainable supported living services.
Conclusion
CQC registration for supported living does not fail because providers lack good intentions. It fails when the service model, documents, and daily practice tell different stories.
In 2026, CQC expects supported living providers to understand one core principle: housing and care must remain genuinely separate. Personal care triggers regulation. Tenancy rights protect independence. The Real Tenancy Test determines whether your service qualifies as supported living or falls into a different regulatory category altogether.
Providers who succeed do three things well. They design services around real choice and control. They prepare evidence that reflects how the service actually operates. And they lead with clarity, not assumptions, when dealing with regulation.
Registration is not just an approval step. It sets the framework for future inspections, CQC reports, and long-term credibility with commissioners and families. When you get the foundations right, compliance becomes easier, inspections become predictable, and your service earns trust over time.
Supported living works best when it feels like home, not a service setting. Build your model around that truth, and the registration process stops being a barrier and starts becoming confirmation that you are doing it right.
Get Expert Support With Your CQC Supported Living Registration
CQC registration for supported living leaves little room for error. One inconsistency can delay your application for months or push your service into the wrong regulated activity.
Care Sync Experts supports supported living providers across England with end-to-end, regulation-led registration support. We focus on clarity, consistency, and evidence—so your application stands up to CQC scrutiny the first time.
How we help supported living providers
- Real Tenancy Test assessment to confirm your model is genuinely tenancy-based
- Statement of Purpose written to reflect personal care only and clear housing-care separation
- Policy and procedure packs tailored to supported living (not generic templates)
- Business plans and financial viability statements aligned with CQC expectations
- Right Support, Right Care, Right Culture compliance for learning disability and autism services
- Fit person interview preparation for Registered Managers and Nominated Individuals
- Post-registration readiness to support strong first inspections and CQC ratings
We also support registrations with Care Inspectorate Wales (CIW) and RQIA in Northern Ireland for providers operating across the UK.
Book a free consultation to discuss your service model and registration route, before you submit and risk rejection.
This guide reflects CQC requirements as of January 2026. Always check current guidance before submitting your application, as requirements can change.
FAQ
What are the 5 CQC standards?
The Care Quality Commission assesses services against five core standards, often called the five key questions. These standards apply across health and social care, including supported living and care homes.
The five CQC standards are:
Safe – People receive care that protects them from harm and abuse
Effective – Care achieves good outcomes and follows best practice
Caring – Staff treat people with dignity, compassion, and respect
Responsive – Services meet people’s needs and adapt when those needs change
Well-led – Leadership promotes quality, safety, and continuous improvement
CQC uses these standards during inspections, registration assessments, and when deciding enforcement action.
How does CQC work?
CQC works as an independent regulator of health and social care in England. Its role is to make sure services meet legal and quality standards.
In practice, CQC works by:
– Registering providers before they deliver regulated activities
– Inspecting services to assess quality and safety
– Publishing inspection reports for public transparency
– Rating services where applicable
– Taking enforcement action when standards are not met
CQC gathers evidence through document reviews, site visits, staff interviews, and feedback from people who use services. It then judges services against its regulatory framework and legal requirements.
What are the benefits of CQC registration?
CQC registration brings both legal protection and strategic benefits.
Key benefits include:
– Legal authority to deliver regulated care
– Increased trust from commissioners, families, and professionals
– Eligibility for local authority and NHS contracts
– Clear quality framework for service improvement
– Published inspection outcomes that support transparency
Well-run services use CQC standards as a management tool, not just a regulatory obligation. Strong compliance often leads to better inspections, stronger referrals, and long-term sustainability.
What are the 5 main components of a care plan?
A good care plan shows how a service delivers safe, person-centred care. While formats vary, strong care plans usually include five core components:
Personal details and background – Who the person is and what matters to them
Assessed needs – Physical, emotional, social, and health needs
Care and support actions – What support is provided, how, and by whom
Risk management – Identified risks and agreed control measures
Review and outcomes – How care is monitored, reviewed, and updated
CQC expects care plans to reflect individual choice, consent, and changing needs, not generic templates.

Leave a Reply